Understanding Malaria: Causes, Symptoms, Diagnosis, and Treatment
1. Introduction to Malaria
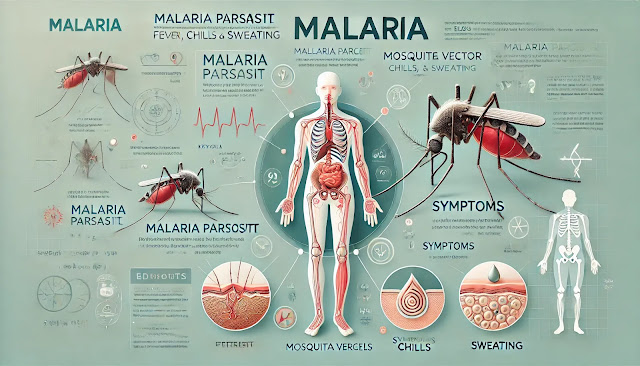
Malaria is a life-threatening disease caused by parasites that are transmitted to humans through the bites of infected female Anopheles mosquitoes. The disease is prevalent in tropical and subtropical regions, particularly in parts of Africa, Asia, and Latin America. If untreated, malaria can cause severe illness and even death. This blog will explore the causes, symptoms, diagnosis, treatment, and prevention of malaria in detail.
2. Definition of Malaria
Malaria is a parasitic infection caused by Plasmodium species, primarily Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale, Plasmodium malariae, and Plasmodium knowlesi. The parasites are transmitted to humans through the bites of infected mosquitoes. Once inside the human body, the parasites travel to the liver, where they mature and infect red blood cells, leading to the symptoms of malaria.
3. Causes of Malaria
Malaria is caused by the Plasmodium parasites, which are transmitted to humans through the bites of infected mosquitoes. The primary causes and risk factors include:
- Mosquito bites: The disease is transmitted when an infected female Anopheles mosquito bites a human, injecting the Plasmodium parasites into the bloodstream.
- Geographic location: People living in or traveling to areas where malaria is endemic are at a higher risk of infection.
- Lack of preventive measures: Individuals who do not use preventive measures, such as insect repellent or mosquito nets, are more susceptible to infection.
4. Symptoms of Malaria
Symptoms of malaria typically appear 10-15 days after being bitten by an infected mosquito. Common symptoms include:
- High fever
- Chills and sweating
- Headache
- Muscle and joint pain
- Fatigue
- Nausea and vomiting
- Diarrhea
- Abdominal pain
In severe cases, malaria can cause life-threatening complications, such as:
- Cerebral malaria: Inflammation of the brain, leading to seizures or coma
- Severe anemia: A significant decrease in red blood cells
- Respiratory distress: Difficulty breathing
- Organ failure: Damage to the kidneys, liver, or spleen
5. Diagnosis of Malaria
Diagnosing malaria requires both clinical evaluation and laboratory tests:
- Blood smear microscopy: A blood sample is examined under a microscope to detect the presence of Plasmodium parasites in red blood cells.
- Rapid diagnostic tests (RDTs): These tests detect specific antigens produced by malaria parasites in a patient’s blood, offering a quicker diagnosis.
- Polymerase chain reaction (PCR): This test detects malaria parasite DNA, providing a more accurate diagnosis in some cases.
- Complete blood count (CBC): A CBC test can show anemia or thrombocytopenia (low platelet count), common in malaria patients.
6. Treatment of Malaria
Malaria is treated with antimalarial medications, and the treatment regimen depends on the type of malaria parasite, the severity of the infection, and the patient’s overall health:
- Artemisinin-based combination therapies (ACTs): ACTs are the first-line treatment for P. falciparum malaria and are highly effective in killing the parasites.
- Chloroquine: Used for treating P. vivax, P. ovale, and P. malariae infections in areas where chloroquine resistance is not present.
- Quinine and doxycycline: These medications are used in cases of severe malaria or when ACTs are not available.
- Primaquine: Used to prevent relapse of P. vivax and P. ovale malaria by killing the dormant liver stage parasites (hypnozoites).
In severe cases, patients may require hospitalization for intravenous (IV) antimalarial treatment and supportive care, such as fluids and blood transfusions.
7. Prevention of Malaria
Preventing malaria involves reducing exposure to mosquito bites and taking preventive medications when traveling to malaria-endemic areas. Key preventive measures include:
- Insect repellent: Use repellents containing DEET or picaridin on exposed skin.
- Mosquito nets: Sleep under insecticide-treated mosquito nets to protect against mosquito bites, especially at night.
- Preventive medications: Depending on the travel destination, taking antimalarial medications like atovaquone-proguanil, doxycycline, or mefloquine can reduce the risk of infection.
- Environmental control: Reducing mosquito breeding grounds by eliminating stagnant water and using insecticides can help lower the risk of malaria transmission.
8. Medications for Malaria
The medications used to treat malaria depend on the parasite species, geographic location, and the patient’s health. Common medications include:
- ACTs: The most effective treatment for P. falciparum malaria.
- Chloroquine: Effective in regions where P. vivax, P. ovale, or P. malariae infections are still sensitive to chloroquine.
- Primaquine: Used to prevent relapse in P. vivax and P. ovale malaria cases.
- Mefloquine: Used both for treatment and prevention, particularly in areas with drug-resistant malaria.
- Atovaquone-proguanil: Used for treatment and prevention of malaria in travelers visiting malaria-endemic areas.
Conclusion
Malaria is a serious parasitic disease transmitted through mosquito bites and can lead to life-threatening complications if left untreated. Preventive measures such as using insect repellents, sleeping under mosquito nets, and taking antimalarial medications are essential in reducing the risk of infection. Early diagnosis and prompt treatment with antimalarial drugs can prevent complications and ensure a full recovery. This blog provides general information and should not replace professional medical advice. For accurate diagnosis and personalized treatment, consult a healthcare provider.



%20where%20a%20person%20stands%20with%20their%20knees%20touching%20while%20their%20feet%20remain%20apart,%20creating%20an%20'X'.png)
.%20The%20image%20should%20depict%20a%20human%20figure%20from%20.webp)



%20in%20a%20medical%20context.%20Show%20symptoms%20like%20constant%20throat%20clearing,%20cough,%20sore%20throat,.webp)
%20in%20a%20medical%20cont.webp)
Comments
Post a Comment